USMLE Step 2 Exam Quiz
USMLE Step 2 Exam Quiz
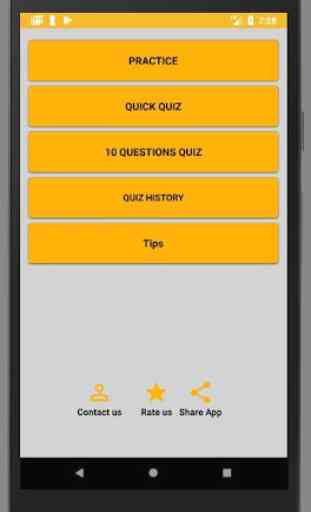
Key Features of this APP:
• At practice mode you can see the explanation describing the correct answer.
• Real exam style full mock exam with timed interface
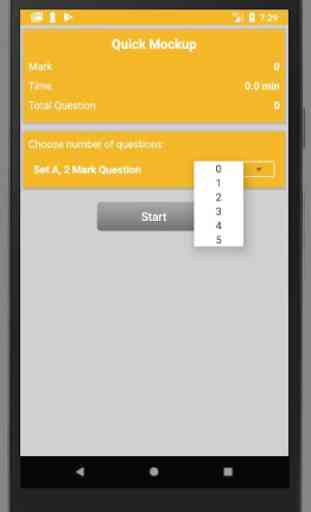
• Ability to create own quick mock by choosing the number of MCQ’s.
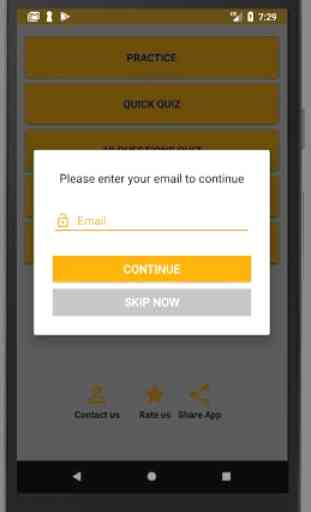
• You can create your profile and see your result history with just one click.
• This app contains large number of question set that covers all syllabus area.
he USMLE Step 2CS exam consists of a series of patient encounters in which the examinee must see standardized patients (SPs), take a history, do a physical examination, determine differential diagnoses, and then write a patient note based on their determinations. The topics covered are common outpatient or Emergency Room visits which are encountered in the fields of internal medicine, surgery, psychiatry, pediatrics, and obstetrics and gynecology. Examinees are expected to investigate the simulated patient's chief complaint, as well as obtain a thorough assessment of their past medical history, medications, allergies, social history (including alcohol, tobacco, drug use, sexual practices, etc.), and family history. Usually, examinees have one telephone encounter, speaking to an SP through a microphone during which there is no physical exam component.
Examinees are allowed 15 minutes to complete each encounter and 10 minutes for the patient note for a single patient encounter. The patient note is slightly different from a standard SOAP note. For the exam note, the examinees will document the pertinent facts relating to the history of present illness as well as elements of the past medical history, medication history, allergies, social history, family history, and physical exam. The examinees will then state up to 3 differential diagnoses relating to the simulated patient's symptoms, and tests or procedures to investigate the simulated patient's complaints.[5] The examinees should also list pertinent positive and negative findings to support each potential diagnosis.[5]The examinees will not recommend any specific treatments in the note in contrast to a true clinic SOAP note (i.e., IV fluids, antibiotics, or other medications). Over the course of an 8-hour exam day, the examinees complete 12 such encounters. Examinees are required to type patient notes on a computer.[6]
USMLE Step 2 CS replaced the former ECFMG Clinical Skills Assessment (CSA) effective June 14, 2004. The last administration of the ECFMGClinical Skills Assessment (CSA) took place on April 16, 2004. When the CSA first started it was strictly for Foreign Medical Graduates while US graduates were not required to do it. That was considered a double standard in the US medical licensing process. Later the CSA was replaced with the USMLE step 2 CS and became inclusive to all medical graduates.
Key Features of this APP:
• At practice mode you can see the explanation describing the correct answer.
• Real exam style full mock exam with timed interface
• Ability to create own quick mock by choosing the number of MCQ’s.
• You can create your profile and see your result history with just one click.
• This app contains large number of question set that covers all syllabus area.
he USMLE Step 2CS exam consists of a series of patient encounters in which the examinee must see standardized patients (SPs), take a history, do a physical examination, determine differential diagnoses, and then write a patient note based on their determinations. The topics covered are common outpatient or Emergency Room visits which are encountered in the fields of internal medicine, surgery, psychiatry, pediatrics, and obstetrics and gynecology. Examinees are expected to investigate the simulated patient's chief complaint, as well as obtain a thorough assessment of their past medical history, medications, allergies, social history (including alcohol, tobacco, drug use, sexual practices, etc.), and family history. Usually, examinees have one telephone encounter, speaking to an SP through a microphone during which there is no physical exam component.
Examinees are allowed 15 minutes to complete each encounter and 10 minutes for the patient note for a single patient encounter. The patient note is slightly different from a standard SOAP note. For the exam note, the examinees will document the pertinent facts relating to the history of present illness as well as elements of the past medical history, medication history, allergies, social history, family history, and physical exam. The examinees will then state up to 3 differential diagnoses relating to the simulated patient's symptoms, and tests or procedures to investigate the simulated patient's complaints.[5] The examinees should also list pertinent positive and negative findings to support each potential diagnosis.[5]The examinees will not recommend any specific treatments in the note in contrast to a true clinic SOAP note (i.e., IV fluids, antibiotics, or other medications). Over the course of an 8-hour exam day, the examinees complete 12 such encounters. Examinees are required to type patient notes on a computer.[6]
USMLE Step 2 CS replaced the former ECFMG Clinical Skills Assessment (CSA) effective June 14, 2004. The last administration of the ECFMGClinical Skills Assessment (CSA) took place on April 16, 2004. When the CSA first started it was strictly for Foreign Medical Graduates while US graduates were not required to do it. That was considered a double standard in the US medical licensing process. Later the CSA was replaced with the USMLE step 2 CS and became inclusive to all medical graduates.
Category : Education

Related searches